How can I get more omega-3 into my diet and how much difference will it make to my health?
Many people worry about eating fat, worrying it will clog up their arteries and lead to weight gain. But fat is an essential part of our diet, and there are some fats that our bodies need. Fats form an important part of every cell in our bodies, where they help ensure that our cells communicate with each other, which means our bodies can function as they should.

Ideally, we need a balance of fats in our diet to ensure the balance of fats in our cells is maintained. But in the West, we tend to have an imbalance of what are called omega-3 and omega-6 fats. This is because we eat too much of the omega-6 fats – these fats primarily come from vegetable oils such as sunflower oil, corn oil and soy bean oil, and they crop up in all kinds of food we eat regularly, mainly processed foods like pastries and cakes, biscuits, crisps, snacks, take-aways, ready meals, some breads, margarine & even breakfast cereals.
At the same time, most Westerners are deficient in omega-3 fats. These fats are anti-inflammatory, help prevent irregular heartbeats, help ensure healthy blood clotting, and reduce the build-up of fat in our arteries; for these reasons, they’re seen as a good way to lower the risks of having a heart attack or stroke. Not having enough omega-3 and having too many omega-6 fats can actually heighten the risk of heart disease, stroke and diabetes. So it’s important that we eat the right amount of omega-3 to help maintain healthy levels of fat in our bodies.
The main source of omega-3 is oily fish, which is why the government recommends we eat fish at least twice a week, with at least one meal being an oily fish like salmon, mackerel, sardines, anchovies or herring.
For those who don’t eat fish, there’s always the option of omega-3 supplements. But some scientists have questioned whether these can provide you with enough omega-3, or as much as you’d be getting from eating oily fish.
So which is the best way to make sure you’re getting the omega-3 you need to keep you in tip-top health – oily fish or omega-3 supplements? And how much difference can taking either of these actually make to your health?
Our experiment
We recruited 60 volunteers from the Liverpool area to take part in an 8 week trial.
The first thing we did was conduct an exhaustive range of tests on each volunteer. One of the key tests we conducted was measuring their omega-3 Index – this is a blood test that measures the amount of omega-3 fats in your red blood cells. It’s seen as a good guide for how much omega-3 fat you have in your body overall, and it’s calculated as a percentage of the total fats that you have in your blood cells.
We also used an ultrasound scanner on our volunteers to measure the thickness and stiffness of their arteries and the efficiency of their blood flow, and we put them through cognitive assessments to see if their mood or attention span would change, as there is good evidence to suggest omega-3 can benefit both. And we took blood and urine samples to test for inflammatory markers amongst other things.
Once we’d done these tests, we divided our volunteers at random into 3 groups and asked each group to follow a specific diet:
- Group 1 would eat oily fish
- Group 2 would consume an omega-3 supplement
- Group 3 was our control – or placebo group
However, because we didn’t want our volunteers to know where their omega-3 was coming from, we had to get a bit sneaky. So we asked each group to do something else regularly:
- Group 1 would be asked to take a daily capsule; which was nothing more than a placebo pill
- Group 2 were asked to eat non-oily white fish twice a week, which has low levels of omega-3
- Group 3 would eat white fish and a placebo pill; so they were getting little to no omega-3
This way, each volunteer was eating fish twice a week, and taking a daily capsule; but none of them knew which group they were in, or what the other groups were getting. We provided them with fish meals to eat twice weekly, and it was an entire meal – this way we would be sure that everyone was having an identical amount of macronutrients (carbohydrate, protein and the different kinds of fats). The only difference between the meals was whether they contained oily fish or white fish.
Because our trial was only running for a set number of weeks, we decided to give our volunteers a high but safe amount of fish or supplements; they were eating about 240g of fish in their meals, and the supplements contained 1500mg of omega-3 (a combination of the key fats – EPA + DHA). Scientists regularly do this if a trial is very short in length, just to see if the intervention/treatment has ANY effect. If not, then it suggests the treatment doesn’t work – if so, then it can be inferred that a smaller dose over a longer period would have similar effect.
At the end of the experiment, we ran all the tests again to see if anything had changed.
Results
One of our key measures was the participants’ omega-3 index. An omega-3 Index of 3% or below is thought to put you into a ‘High Risk’ category for heart attacks and strokes; an Index between 4-8% puts you at ‘Moderate Risk’, whereas an omega-3 Index of 8% or above means you’re at ‘Low Risk’.
All our volunteers had a fairly low omega-3 Index when the trial started – each group was around 4-5%, but some individuals were as low as 3%. So at the start of our trial, many volunteers were at a moderate to high risk of serious illness.
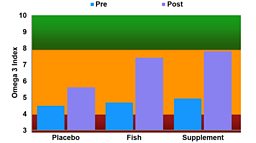
After the trial, it’s a different story. The oily fish group and the omega-3 supplement group all leap to 7 - 8%, meaning they’re heading towards the low risk category.
There was a very slight but statistically insignificant improvement in our control group, which scientists put down to the fact they were probably eating a slightly healthier diet than they normally might. Whether it was the two fish meals a week we gave them (which had very little omega-3, but also had very little omega-6, plenty of vegetables and fibre), OR because their participation in our test had prompted them to eat generally more healthily, this slight improvement is likely down to improved overall diet. However, their improvement was in no way scientifically significant.
Many of the other tests we did came back with mixed results, but this is probably because the trial length was too short. For example, it was unlikely that we would see a change in arterial thickness or stiffness in our timeframe.
What this means
Our trial suggests that oily fish and omega-3 supplements are both good at providing your body with omega-3 fats – in our limited timeframe the omega-3 fat levels in the blood cells of all the volunteers in those groups increased for the better.
For some of them it moved them from the High Risk to the Low Risk category, which is very encouraging.
Were they to sustain this diet over a longer period of time they might all move into the low risk category for serious illnesses like heart disease, stroke and diabetes.
Even though we were giving people higher doses than you might normally take, the reality is, if you took lower doses over a longer timeframe – or incorporated omega 3 into your lifelong diet – then you’d likely see similar improvements.
What’s more if you choose to get your omega 3 from oily fish, there are other benefits – fish is a great source of lean protein, and you’re also getting a range of vitamins and minerals.
If you really don’t like fish and would rather take supplements, take a look at our advice on what to look for when you buy them.
Ultimately, the choice is yours, but one thing is clear – we could all do with more omega-3 in our diets if we want to cut our risk of serious illness.
Should I buy omega 3 supplements?
We took ten different omega 3 supplements and sent them to for testing. We wanted to know whether the supplements contained what they said they did, whether any of the oil had gone rancid and whether they offered value for money.
The two main omega-3 fats you need to get from your diet are EPA and DHA. Depending on which health organisation you believe, we should be having at least 200mg to 450mg of these fats combined every day. We found that all of the supplements we tested did contain the amounts of EPA and DHA they said they did, and that these levels were all above 200mg. However we found that these supplements came at wildly different prices – depending on which brand you bought you could be paying anything from £13 a year to over £300 a year to get your recommended levels.
We also found that one of the oils had gone rancid despite the fact that it was well within its use by date. Many things can cause oil to turn rancid including exposure to air and light.
So if you want to buy supplements our advice would be:
- Check the label to ensure that the supplement contains enough DHA and EPA.
- Check the use by date and pick a supplement that has plenty of shelf life left.
- Look for accreditation badges as brands that have sought accreditation are likely to have good quality control in place.
- Look out for supplements that contain antioxidants as these can help protect against the oil going rancid.
- Store your supplements in a cool dark place and keep the lid tightly closed. You may also want to choose smaller bottles so that the capsules are exposed to light and air for shorter periods of time once opened.
More about our experts
More about essential fatty acids
Recipe ideas
-
![]()
Oil-rich fish (or oily fish) are those that have oil distributed through their body, as opposed to white fish, whose main concentration of oils is located in the liver.