Fears some ambulances 'left Covid patients at home'
- Published
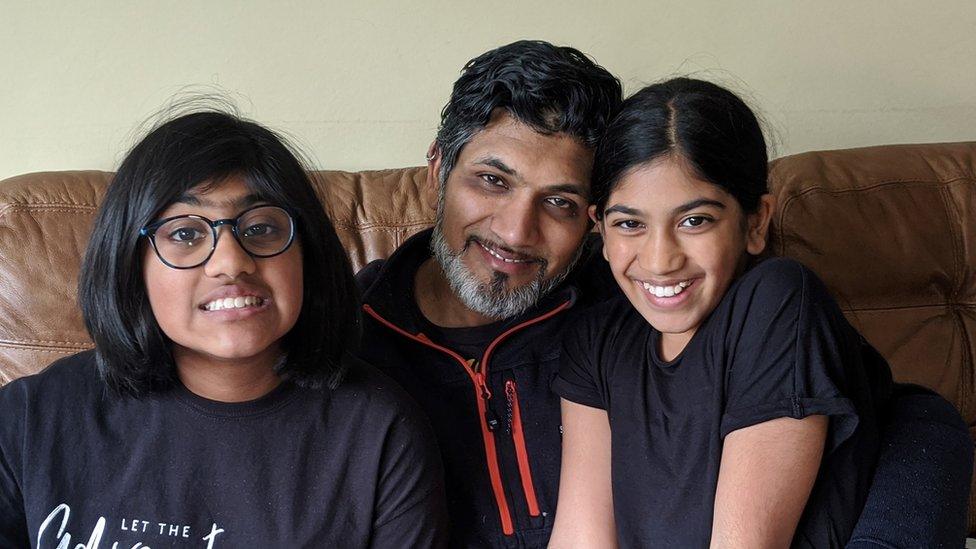
Anand Punja and his daughters
Some seriously-ill Covid-19 patients in London may not have been taken to hospital by ambulance because of a system temporarily used to assess people, a ģÉČËŋėĘÖ investigation suggests.
Patients could have "become very sick or died at home" instead, a paramedic claimed.
One family said they had to plead to get hospital care.
The London Ambulance Service (LAS) says it keeps its systems for assessing patients under review.
Medical professionals use a scoring system, called 'NEWS2', as one way of identifying patients at risk of deteriorating, a check normally used for sepsis patients.
Under normal circumstances, ambulance teams would blue-light anyone with a score of five or above to hospital.
But on March 18, LAS workers were told to apply the NEWS2 check to suspected Covid patients - and that many of those with a score up to seven could be "suitable for community care", even if there were issues with breathing rate, oxygen supply and consciousness.
LAS said the system of checks it used reflects evolving understanding of how the disease progresses to identify those at risk of deteriorating.
Other assessment tools are used by ambulance crews, who are also expected to use their own clinical judgement.
'Suddenly became very sick'
But one paramedic, who wanted to remain anonymous because she did not have permission to speak to the media, said she believed that as a result of the NEWS2 advice, crews went to patients "who may have been seen by ambulance before and then suddenly became very sick or even just dropped dead."
The LAS directive came just one day before Northwick Park, a major north-west London hospital that has struggled with the volume of coronavirus patients it has received, declared a major incident and said that its critical care unit was full.
Over the Easter weekend, the LAS changed its guidance to say suspected coronavirus patients with a wider range of symptoms and a much lower NEWS2 score of three to five should be taken to A&E for assessment.
A LAS spokesman said: "We are constantly updating our guidance to staff to better reflect the national understanding of this new disease and ensure we always provide the best advice for our patients' health, and that of our staff."
Anand's story
Sital Punja, from north west London, said she had to plead with paramedics to admit her husband to hospital when his Covid-19 symptoms worsened.
Anand Punja, 45, was fit and healthy before he contracted coronavirus.
But on March 30, day eight of his illness, he was struggling to breathe.,
The family spoke to NHS111 and a GP who recommended calling an ambulance.
But the paramedics refused to take him to hospital, even though Anand's oxygen saturation level was 92% - when it should be 96-98%,
Mrs Punja said: "The paramedics said he was fine and that I should just give him paracetamol and water."
But two days later he was unable to get from the bed to the toilet and was begging for oxygen, so she called 999 again
"I waited three hours for an ambulance. The paramedics were the same two people as the previous visit. They said that they had been there before and they didn't need to assess him.
"I asked what it would take for him to be admitted and they said that he would need to be blue lipped and in cardiac arrest."
She said that, even though her husband was then taken in, the experience of having to persuade them was traumatic. "It's just playing a lottery with lives."
He was in hospital for five days and needed intravenous antibiotics and oxygen.
LAS said patient confidentiality meant they could not comment on the case.
An emergency medicine doctor, who also wanted to remain anonymous, said that the NHS in London had capacity for seriously-ill patients and that it was a concern that his hospital had seen fewer of them.
"We were surprised over those weeks that the emergency department was not as busy as we thought it would be, and overall patient attendances were low," she said.
"At the same time we, as emergency department staff, became aware of the rules implemented by the LAS where they were not bringing possible Covid patients into hospital unless they had an early warning score of seven or above.
"This means that many potentially sick patients have been left at home to deteriorate."
A spokeswoman for the GMB union which represents some ambulance personnel said: "Never before have our ambulance members faced a challenge like Covid-19. We're beyond proud of them.
"They have handled the pressure put on both them and their families with courage, professionalism and determination."
Trisha Greenhalgh, professor of primary care health sciences at Oxford University, and an expert in identifying at-risk patients, said NEWS scores were not perfect, or designed for people with Covid, and NHS staff need to use their clinical judgement too.